Adults with Asperger syndrome sometimes find themselves in a twilight land between social, medical and disability supports, where the issues of daily living are neither a ’medical problem’ nor a ’disability problem’ — just like ’normal’ people. Many adults with Asperger syndrome have arrived through other diagnoses first, or have current mental health issues (comorbidities). Formal supports tend to assume one primary need, such as disability support if IQ is below a threshold of 70 or mental health services when psychiatric symptoms are deemed clinically significant. The formal supports are not integrated, may prohibit access to more than one service and address social issues through their own re-interpretations. Medication can be very helpful, but can also be used as a substitute for supporting the life issues that are causing difficulty.
TLDR? This is a rant.
Life is distressing
Psychiatrists only see people who are, or have a history of, serious distress. But never forget that life is full of distress, and not all of it is bad — vigilance, anxiety and panic keep us from being eaten by wolves and push us to achieve goals. Ian Dury (“crippled with polio” in real life) sings about a boy who “will die cos I’m crippled with nerves” at the thought of approaching a girl he fancies. This is normal, until a psychiatrist views the isolated symptoms through the microscope of the Diagnostic and Statistical Manual of Mental Disorders (DSM), losing all sight of the context in which those symptoms arose.
Social stressors could be any issue, negative or positive — and positive change can be just as stressful as negative events. Some example stressors are falling in or out of love, moving house or changing jobs — the Holmes-Rahe stress scale lists the most stressful events rated by adults and students. In my own case, the biggest current stressor in my life right now is that I chose to submit a document to the Independent Inquiry into Child Sexual Abuse (the Goddard Review). This process has taken many months, is extremely stressful and involves writing emotionally difficult material in formal language. Police and lawyers are involved, along with the risk (at least in my paranoid mind) of being sued for libel if I get even one word wrong. There is always social stress, usually less severe and long-running than this process.
Labels and diagnostic boxes
My own diagnosis with Asperger syndrome followed treatment for depression, PTSD, psychosis and self-harmful behaviour. I must emphasis that I was diagnosed with Asperger syndrome because I had a mental health crisis, and had never received support of any kind previously, although I would probably have benefited throughout my life. A mental health crisis, triggered by bullying, job loss or other stressors is the most frequent route to a diagnosis in adulthood. The ASPECT Report by Luke Beardon and Genevieve Edmonds in 2007 found that “68% of individuals have had contact with Mental Health services; Of those only 12% found it a positive experience; Of those who have had contact with Mental Health services 10% did so as a result of attempted suicide or following suicidal thoughts, 38% for depression, and 12% for anxiety. There is still clearly a lack of understanding of AS in MH services as a whole.” They also report that 28% of adults have a concurrent diagnosis with at least one other condition (dyslexia, dyspraxia or AD(H)D) and most found the route to diagnosis difficult. The Sheffield Asperger Needs Survey found that “61% of people indicated that they had some form of psychiatric difficulty. 53% indicated that they suffered from anxiety, 45% from depression, 17% from suicidal thoughts, 26% from panic attacks, 3% from schizophrenia, 8% from psychosis, 17% from an obsessive-compulsive disorder, and 16% from some other condition.”
Other studies state that at least 50% of people with Asperger syndrome experience depression (Baron-Cohen, 2008). Two thirds of people with Asperger syndrome exceed the threshold for alexithymia (Samson et al, 2010), and there is probably a higher rate of anorexia nervosa (Baron-Cohen et al, 2013) and bulimia (Tchanturia et al, 2013). Psychiatrists often ask questions about mood and feelings that are alien and unanswerable to people who do not have a strong emotional vocabulary, who would be better served by questions about specific behavioural changes (why ask about ’appetite’ when you could ask about weight change?).
The cross-over between psychiatric disorders cannot be stressed enough — the DSM-5 diagnostic criteria for Autism Spectrum Disorder include behaviours in common with OCD, AD(H)D, schizophrenia and other diagnostic categories. (Boschloo et al 2015 has a beautiful illustration of diagnostic crossover in Figure 1). These diagnostic categories have become boxes that frequently include words like “These disturbances are not better explained by …”, which gives the (false) impression that a person can not be diagnosed with two or more things at the same time. Such comorbidities affect the majority of autistic people, but health services are geared towards handling ’the primary diagnosis’, or whichever diagnosis is predominating at some point in time or space. There can be a long waiting list to switch from one service to another when the predominanating diagnosis changes. This change may be in time and space (by changing jobs or relationships) which changes the significance of symptoms or traits, even though there is no change in the underlying conditions.
Medication as a ’cure’
There is no medication to cure or treat autism. The NICE guidelines (CG170 for children CG142 for adults) state “Do not use pharmacological or exclusion dietary interventions for the management of core features of autism in children and young people . . . Consider antipsychotic medication for managing behaviour that challenges . . . Offer psychosocial and pharmacological interventions for the management of coexisting mental health or medical problems” and the CDC states “There are no medications that can cure ASD or treat the core symptoms. However, there are medications that can help some people with ASD function better. For example, medication might help manage high energy levels, inability to focus, depression, or seizures.” (CDC Autism Spectrum Disorder Treatment). This should mean that people with autism are treated for mental health as and when they occur, like other people with mental health conditions.
I use medication for anxiety and to avoid panic, as well as occasional medication to control intrusive and perseverating thoughts. These medications are effective and extremely beneficial to me — especially, for instance, in controlling anxiety when travelling or dealing with distressing, intrusive thoughts. However, psychiatrists tend to take my expressions of my life experience, reformulate it into their concepts of symptoms, map those into one of their (mutually-exclusive) diagnostic boxes and then modify my prescription to match their experience of that boxful of patients. Over the past fifteen years I have had my prescription modified to include:
Amitriptyline, Anafranil, Anxicalm, Buscopan, Clonactil, Diazepam, Effexor, Gamanil, Largactil, Librium, Lithium carbonate, L-Tryptophan, Lustral, Lyrica, Mefanamic acid, Mirtazapine, Mobic, Priadel, Quetiapine, Sertraline, Spasmonal, Stilnoct, Tradol, Venlafaxine, Xanax, Zimovane
— for Depression, Anxiety, Psychosis, Abdominal pain, Sleep

Many of these medications have been increased and increased in dose until the side-effects were intolerable, and then replaced with an alternative — most were not effective in producing the outcome expected by the psychiatrist. In-patient medication included synergistic treatment with antihistamine to increase the potency of antipsychotic, anti-anxiety and sleep medication (the “triple-whammy” chemical cosh). Most in-patients were given a ’mini-Guinness’ of antacid suspension poured over syrup of figs for the inevitable constipation caused by these medications combined with lack of physical exercise in a closed ward. (Weight-gain was an average of 3 kg per month of in-patient confinement, excluding those on weight-gain programmes).
One psychiatrist with what I can only describe as a personal obsession with hypnagogic psychosis, reframed everything I said into a framework that supported this as my diagnosis and prescribed medication appropriate for this imagined condition. Needless to say, neither my condition nor the psychiatrist’s improved.
Psychiatrists need to be aware that “Autism is a lifelong neurodevelopmental condition, the core features of which are persistent difficulties in social interaction and communication and the presence of stereotypic (rigid and repetitive) behaviours, resistance to change or restricted interests. The way that autism is expressed in individual people differs at different stages of life, in response to interventions, and with the presence of coexisting conditions such as learning disabilities (also called ’intellectual disabilities’). People with autism also commonly experience difficulty with cognitive and behavioural flexibility, altered sensory sensitivity, sensory processing difficulties and emotional regulation difficulties. The features of autism may range from mild to severe and may fluctuate over time or in response to changes in circumstances.” (NICE CG142)
Right now, and for the past year, my life-stressor is causing me difficulty with night-time wakefulness, intrusive negative thoughts and feelings of persecution. These are entirely normal responses to reviving memories of deeply unpleasant events in my past, and of interacting with current events that are thoughtlessly inhumane (I had one telephone call to say that “The Chief Inspector is on the line”, although he only asked me to confirm my date of birth — “I’ll die cos I’m crippled with nerves” comes to mind). I actually would not dare to tell my psychiatrist a fraction of the thoughts that I have, in case they are reframed as paranoia, delusions, a persecution complex, personality disorder or self-harmful intentions.
Unicorns everywhere

(This is the constellation of stars known as Monoceros, the Unicorn. It is not a real unicorn.)
There are several problems in seeing life experience as isolated symptoms thought the microscope of psychiatry. All of them tend towards seeing (all aspects of) life as a disease, or a constellation of disease symptoms, and then to medication of social issues. This is a technical attempt to solve a complex social issues (like putting up CCTV cameras to ’solve’ crime). These problems come from reframing the ’problem’, as expressed by the patient, into ’solutions’ that the medic has competence in or authority over — such as access to hospital or prescription medication. Everyone wants to feel wanted and useful, so it is natural and human to reframe the patient’s expressions into a need that the professional can solve. Reframing has other consequences:
Firstly, the medical solution may solve only a part of the need as perceived by the patient. Secondly, medication (in particular) may go too far in over-solving an issue — controlling anxiety or obsessive thinking often results in major tranquillisation and loss of capacity to think clearly — which may be desirable if there is a risk of self-harm, but completely unproductive (as in my case) if the anxiety is caused by the need to produce complex and emotionally upsetting documents. Thirdly, reframing may simply be wrong — seeing autistic perseveration as OCD, or intrusive thoughts as delusional ideas of reference, or sensory overload as hallucination — the treatment (anti-psychotics) might reduce the ’symptom’, but at great cost if it is part of the “lifelong neurodevelopmental condition” that is the patient’s identity.
The psychiatrist’s microscope, seeing one symptom, or even an approximation of a constellation, is liable to see the entire unicorn behind Monoceros. A person who seeks help with difficulty sleeping becomes an insomnia patient, insomnia becomes a component of a larger diagnostic category, other elements of the patient’s expressions and history add weight to the diagnosis and suddenly you are the unicorn made flesh. Inviting a medical professional to advise over sleep is inviting professionalism into the bedroom, with the psychiatrist’s authority over every aspect of life, and a consequent loss of capacity to make decisions and loss of the right to consent or refuse treatment. (My own childhood history intertwines with this uninvited domination of my capacity and consent particularly in a horribly delicate way).
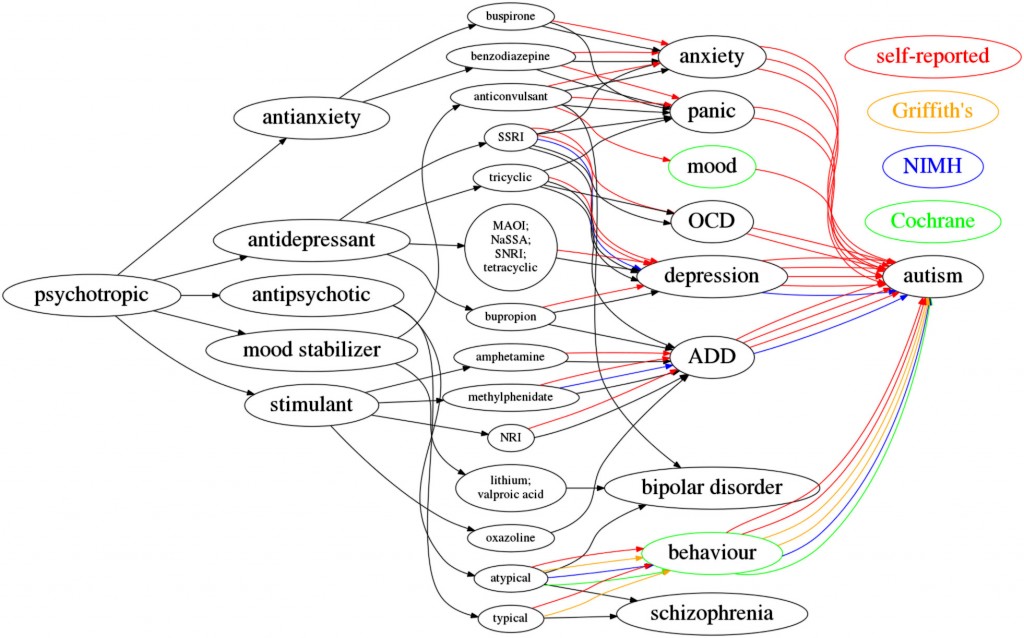
In an informal set of data-gathering, people reported use of every category of psychotropic medication for autism, not for allied medical conditions. The network above shows that some people reported using the atypical antipsychotic Aripiprazole for symptoms of autism, as recommended (for short-term use) by both Cochrane (Cochrane: Aripiprazole, Cochrane: Risperidone) and the NIMH. The NIMH additionally suggests fluoxetine and sertraline for depression, anxiety, repetitive behaviours and aggression, as well as methylphenidate (Ritalin) for ADHD. These are the green and blue lines in the diagram. The red lines are self-reported use of prescription medication that is outside guideline treatment, and often (the ’behaviour’ node) an off-label use of psychotropic medication to control behaviour that challenges family members or challenges the professional.
Psychiatric power and encroachment
The psychiatric care that I have had, especially as an inpatient, has been provided by people who largely have excellent skills and professionalism. The service as a whole, especially as an outpatient, is not even mediocre. It is poor. For instance it is not unusual to be one of thirty people with an appointment at the same time, like livestock awaiting dipping; to wait three hours before being seen; to have an ’emergency’ appointment within a week or more; to not know the name of the latest harried registrar; to be seen by someone new who has no access to your medical history; to be mistaken (personally and diagnostically) for someone else; or to be seen in surroundings that are crumbling. The mental health system is overloaded and underfunded. and people with low-priority, low-intensity or occasional needs who do not present an immediate danger are not appropriately served. People with chronic or “lifelong neurodevelopmental condition” are habitually badly served because there are few, if any, consequences. I am frequently amazed by the caring individuals who work within the system (public, private and caritable) who maintain incredible humour, dignity and compassion under duress within a service starved of essential resources.
There is personal inadequacy and poor training in the system. Non-urgent outpatients are reviewed by registrars and trainees (perhaps only once with any one professional), and not by not consultants with whom they have a relationship. Incompetent staff can misuse their power — the trainee who wrote “NC/NA” (“non-compliant / non-attender”) on my folder after I questioned inappropriate treatment, which affected treatment by other staff for the next four years; the registrar who scheduled each appointment in a different building; the trainee who said “autism is developmental, but you aren’t a child”; the trainee who said “the side-effects of these (psychiatric) medications are trivial compared to chemotherapy”; the trainee who said “I can’t take your word for it, I will need to check with the consultant” (now retired); the psychiatric nurse who told me that I had “sinned against our Lord Jesus Christ” by harming myself, and then denied saying it when challenged; or the registrar who applauded diagnosis-streamed appointment groups, but said “the drugs are just the same”.
In a couple of shocking papers, psychiatric professionals describe semi-formal structures of coercion and control. Choudhury et al (2015) equate maturity and acquiescence with a medication protocol — irrespective of pharmocological efficacy, compliance is described in terms of responsibility, growth and emotional intelligence. Valenti et al (2015) state that psychiatric professionals are ’uncomfortable’ with informal (and therefore unregulated) coercion, yet frequently employ persausion, interpesonal leverage, inducements and threats. Over the past fifteen years I have experienced tests of acquiescence and coercion including — the threat of electro-convulsive therapy (ECT) or more sedating medication; threats of transfer to another unit; the actual withdrawal of service, after my refusal to sign a written ’confession of distrust’ in a professional’s decision; the threatened and actual disclosure of personal details to family members; the threat of longer confinement in a locked ward; and the threat of involuntary admission (sectioning) if I did not take my medication “in a compliant manner” or “show appropriate deference”.
More than anything, more than any of these single episodes, the problem is the encroachment of a medical view of my problems into my life and choices. I am obliged (as a public health service patient) to attend regular reviews, at which trainees and registrars ask intimate questions about every aspect of my life and beliefs. I am obliged to answer them truthfully and to comply with their instructions outside the consulting room — I remain a patient outside of their domain, or rather their domain encroaches into every aspect of my life. Not complying is not an option, unless I leave the system and risk non-treatment in any future crisis.
Social solutions to social problems
Ranting about the mental health service is not, in itself, productive and I want to emphasise again that psychiatric medication has been extremely beneficial to me (although not all of it). It is productive to look at how problems that are essentially social are reframed with psychiatry, decontextualised and treated as isolated symptoms or symptom constellations. My interactions with the Goddard review has caused me to re-experience some past events with powerful immediacy, and the emotions (which I struggle to recognise) cause significant interference in the present. My sleep and concentration are affected, sometimes very severely. I have needed (and have no access to) help in writing a difficult submission — although, of course, I also lack the personal skills to identify or ask for help which is available (I have access to a social worker, but did not realise it was appropriate to trouble the service). I have only been offered medication, or changes of medication (four changes of prescription this year), with tranquilizing effects that interfere with writing the document that causes the symptoms. The treatment has been, to be polite, sub-optimal.
The whole concept of ’feelings’ and ’emotions’ is hard for many people with autism. “How do you feel” only has one appropriate, learned response (“fine”), but the psychiatrist’s concept of mood is being used to guide medication decisions. I often wonder, if I had been diagnosed with Asperger syndrome before any psychiatric condition, would my understanding of autism have prevented some the mental health issues? Would the psychiatrists understanding of autism have meant that some of my issues (such as lack of affect) would not have been perceived (and incorrectly treated) as mental health conditions? Overall, would my mental health have been treated differently or not treated at all (because there is no cure for my autistic deficits)?
I don’t expect the inmates to run the asylum (although it would be nice if more patients / users / clients were promoted to positions where we can dictate the interventions we receive). I do think that psychiatrists are poorly integrated even within their own discipline, let alone externally with disability, health, social and charitable services. This is especially problematic for people with long-term and lifelong conditions. Autism is a “lifelong neurodevelopmental condition” and is not going to respond to the interventions and wishful thinking of every new trainee and registrar, but they all behave like Robin Williams in “Awakenings” (the film is fiction — the book is much less upbeat). The management and care of chronic and lifelong patients is demanding and unrewarding, but patients do feel a huge respect for and benefit from a good physician who can listen, interpret and contextualise their lives.
References
- Balfe, Chen and Tantam (2005) Sheffield Survey Of The Health And Social Care Needs Of Adolescents And Adults With Asperger Syndrome
- Baron-Cohen (2008) Autism and Asperger Syndrome: The Facts. Oxford University Press.
- Baron-Cohen et al (2013) Do girls with anorexia nervosa have elevated autistic traits? Molecular Autism, 4:24
- Beardon and Edmonds (2007) ASPECT Consultancy Report: A National Report on the Needs of Adults with Asperger Syndrome
- Boschloo et al (2015) The Network Structure of Symptoms of the Diagnostic and Statistical Manual of Mental Disorders. PLoS ONE 10(9): e0137621
- CDC Autism Spectrum Disorder (ASD)
- Choudhury et al (2015) “Learning how to deal with feelings differently”: Psychotropic medications as vehicles of socialization in adolescence. Social Science & Medicine 143:311e319
- Cochrane (2007) Risperidone for autism spectrum disorder
- Cochrane (2012) Aripiprazole for autism spectrum disorders (ASD)
- NICE (2013) CG142: Autism in adults: diagnosis and management
- NICE (2013) CG170: Autism in under 19s: support and management
- NIMH Autism Spectrum Disorder
- Samson et al (2012) Emotion Regulation in Asperger’s Syndrome and High-Functioning Autism. Emotion, 12(4):659-665
- Tchanturia et al (2013) Exploring autistic traits in anorexia: a clinical study. Molecular Autism, 4:44
- Valenti et al (2015) Informal coercion in psychiatry a focus group study of attitudes and experiences of mental health professionals in ten countries Social Psychiatry and Psychiatric Epidemiology, 50(8):1297-1308
Hello, just signed up for your blog following your Tweet to me re. Lancet abstract. This post is brilliant. I’m wondering if you would be ok with me showing it to my Mental Health Coordinator ? I was diagnosed this year,aged 48, with ASD (Aspergers).Previously diagnosed as Bipolar. and still on 2 mood stabilisres & one antidepressant ( 10 years on current regime). I will shortly have an appointment with what will be the third locum psychiatrist in less than a year! My ASD diagnosis happened through my own insistence to being assessed. I’m one of the many who had the ‘Eureka moment’ whilst researching to help other family members – concerns for both my sons since diagnosis of several other,younger, relatives. I relate very strongly with your experiences with MH srvices & wnat to say Thankyou for writing this post. I am wondering if you ,and others, had similarly difficult experiences with Psychologists too ( from the psych o’therapeutic’ angle rather than the psychiatric angle). The parallel ( the irony) comparison would be very interesting to read about, if you and/or others have written about this . All the above referring to misdiagnosis / underdiagnosis /missed diagnosis. I’m not an academic, I’m processing, reframing etc. Thankyou :o)
Yes, you are welcome to refer to the blog post.
My own experience of diagnosis was similar. I was diagnosed in 2008, aged 44, after several years of unproductive treatment for depression, anxiety, PTSD etc – my response to the drugs was not the ‘return to healthy affect’ that the psychiatrists expected. A fantastic psychologist suggested ASD and the multi-D team formally assessed me and agreed. Life has been a whole lot better since diagnosis, without all the antidepressant and antipsychotic drugs (and continuous experimentation).
Counselling and CBT were, at times, awful without the ASD diagnosis. I can’t answer the “how do you feel” questions, or explain motives in emotional terms – I think I do things for pragmatic outcomes, not feelings. Counselling with an ASD specialist has been good.
Perhaps I will write something about psychotherapy sometime.
Thankyou,this will be useful to share. I’m so glad your Psychologist had the wisdom to suggest ASD assessment. It’s really helpful for me to see people having positive experiences with MH professionals, but particularly Psychologists. Indeed, the Psychologist I saw this year supported my request to be referred for ASD assessment . It took a lot for me to see her initially, but I’m glad I did ( Before my Bipolar diagnosis I had a terrible experience with a (now retired) psychologist. ) As regards CBT, I couldn’t ( and still can’t) adopt what I saw as flawed logic and huge assumptions. Maybe,like you , I could try it again, with an ASD counsellor, if I find one. Sadly I too have had ‘psychotherapy’ years ago that was deeply traumatic. I don’t believe that will happen again now I have my correct diagnosis, and I need therapy to heal from the ‘therapy’ if you know what I mean. Anyway, to cut my ramblings, I still need to look at the meds situation with the MH team and work out if the Bipolar is a misdiagnosis. I would like to be off all meds too. I know I have suffered severe depression, anxiety and psychotic episodes , but given the trauma of a lifetime of not KNOWING I’m autistic, that is hardly surprising. I know I’m autistic but I seriously question whether I’m also Bipolar. I,m now particularly interested in finding out if there is, or could be, a specific therapeutic process available for late-diagnosed autistics – to heal from the trauma and legacy of not knowing, and to move on to a happier life, with the recognition,supports and accomodations we deserve. That’s probably quite naive of me , but It is my wish. As an extension of this, I hope for a day when nobody gets ‘missed’ .
Just to clarify, I am still using some medication and I think that medication is effective and important. I use medication for generalised anxiety (GAD) and for situations where I am particularly anxious (such as travel). Occasional antipsychotics help deal with very strong intrusive thoughts, but disrupt my life a lot. If the psychiatrist insisted on other therapy, such as antidepressants, then I would almost definitely comply.
My problem, which I was ranting about, is that the very human quest to feel valued leads every trainee and registrar to modify my prescription (usually upwards) in an attempt to improve my functioning. It is necessary to comply or to leave the service, in which case I would face a very long wait to re-enter the system if I ever had a mental health crisis. The evidence is good enough to feel that I am at risk of future depression.